What is Rheumatic Heart Disease?
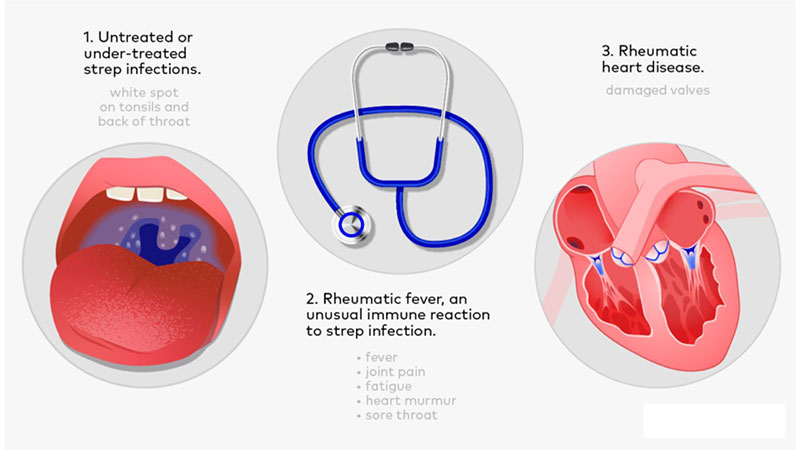
Rheumatic heart disease (RHD) is a long-term heart condition caused by damage to the heart valves following rheumatic fever. Rheumatic fever itself is an inflammatory reaction that can occur after an untreated throat infection caused by group A streptococcus bacteria.
Over time, repeated episodes of rheumatic fever can lead to scarring and deformity of the heart valves, most commonly the mitral and aortic valves. This damage can make it harder for the heart to pump blood effectively and may lead to serious complications if left untreated.
How Does Rheumatic Heart Disease Develop?
Rheumatic heart disease begins with a throat infection such as strep throat or scarlet fever. If this infection is not treated promptly with antibiotics, the body’s immune response can mistakenly attack its own tissues — including the heart valves.
Each episode of rheumatic fever increases the risk of long-term damage. This is why early treatment of throat infections in children and young people is essential to prevent RHD.
Common Symptoms
Symptoms of rheumatic heart disease often appear years after the initial infection. They depend on which valves are affected and how severe the damage is.
Typical signs and symptoms include:
- Shortness of breath, especially with exertion
- Fatigue or reduced exercise tolerance
- Palpitations (awareness of an irregular heartbeat)
- Swelling of ankles or feet
- Chest discomfort or pain
- Fainting episodes (rare)
Some people may remain symptom-free for many years, with RHD only discovered during a routine medical check.
Who is at Risk?
Rheumatic heart disease is more common in parts of the world with limited access to healthcare, but it still occurs in the UK — particularly among people who grew up in regions where rheumatic fever is frequent.
Children aged 5 to 18 are most at risk of developing rheumatic fever after a strep throat infection. Recurrent infections and delayed treatment significantly increase the chance of heart damage later in life.
How is Rheumatic Heart Disease Diagnosed?
Diagnosis is based on a combination of medical history, physical examination and specialised heart tests. These may include:
- Echocardiogram (heart ultrasound): To check valve structure and function
- Electrocardiogram (ECG): To look for abnormal heart rhythms
- Chest X-ray: To assess heart size and signs of heart failure
- Blood tests: To detect past streptococcal infection
Early detection is important, as valve damage can progress silently over time.
Treatment Options
Treatment focuses on preventing further heart damage, managing symptoms, and repairing or replacing damaged valves if necessary.
- Antibiotic prophylaxis: Long-term antibiotics may be recommended to prevent future strep infections and further valve injury.
- Medications: Diuretics, beta-blockers or anticoagulants may be used to manage symptoms or prevent complications.
- Surgery: Severe valve damage may require surgical valve repair or replacement.
- Lifestyle adjustments: Regular follow-up, vaccinations, and good oral hygiene reduce the risk of complications such as infective endocarditis.
Prevention and Long-Term Outlook
The best way to prevent rheumatic heart disease is by promptly treating sore throats in children and adolescents with antibiotics. People with a history of rheumatic fever often need regular medical follow-up throughout life.
With appropriate treatment and ongoing care, most people with RHD can lead active, fulfilling lives. Advances in surgery and long-term medical management have significantly improved outcomes for patients worldwide.