What is pectus excavatum?
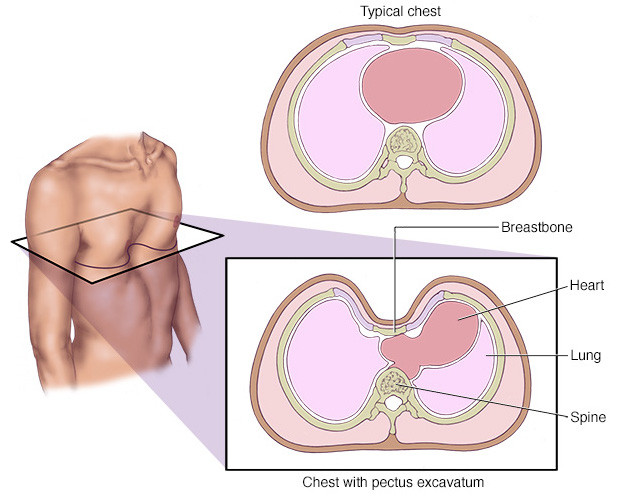
Pectus excavatum, also referred to as sunken chest, is a deformity in the structure of the anterior wall of the chest in which there is an abnormal shape of the sternum (the front chest bone) and the rib cage. This results in a caved-in or sunken appearance of the anterior part of the chest. This anomaly can either be present since birth or it can develop progressively with growth, particularly during the growth spurt typically seen in puberty.
What causes pectus excavatum?
The exact cause of pectus excavatum is unknown. The condition is thought to affect about 20,000 people in the United Kingdom alone. Whereas there is a clear genetic link in many cases, a clear genetic cause, like a particular mutation is not identified in the majority of children. Pectus excavatum can be associated to some syndromes like Noonan syndrome, Marfan syndrome, and Loeys-Dietz syndrome and it can be seen in other children with connective tissue disorders like Ehlers-Danlos syndrome (EDS). Fortunately, the majority of people with this condition will not have an overtly evident abnormal connective tissue problem, but they may have fine features. For example, it is common for people with pectus excavatum:
- to be thin and tall;
- to have had hypermobility of the joints;
- to have joint pains sometimes;
- in some cases they may have a hyperelasticity of the skin and minor abnormalities of the heart valves.
How does pectus excavatum affects children and adolescents?
Even though the majority of children with pectus excavatum have no health consequences, except sometimes for the psychological consequence of having an abnormal appearance of the chest, some children and young adults may experience cardiac or respiratory symptoms. Chest pain and feeling of racing heart (palpitations) are common in children and adolescents with this condition. Some children and adolescents may also develop more severe negative psychosocial effect, and they refrain from undertaking any activity in which they have to expose their chest. Whereas the defect was initially considered to be only of cosmetic importance, it has recently become apparent that it can have an impact on the heart and the lung function and the way their heart and the lung interact with each other.
What cardiac problems can be seen in children with pectus excavatum?
Children and adolescents with this condition may have a floppy appearance of the mitral valve and not infrequently may have minor leakages of the mitral valve (inlet valve on the left ventricle). This usually of no significance and can rarely become a problem. A small minority of people with sunken chest may have significant heart problems, particularly with enlargement of the main body artery which is known as the aorta.
How is pectus excavatum diagnosed?
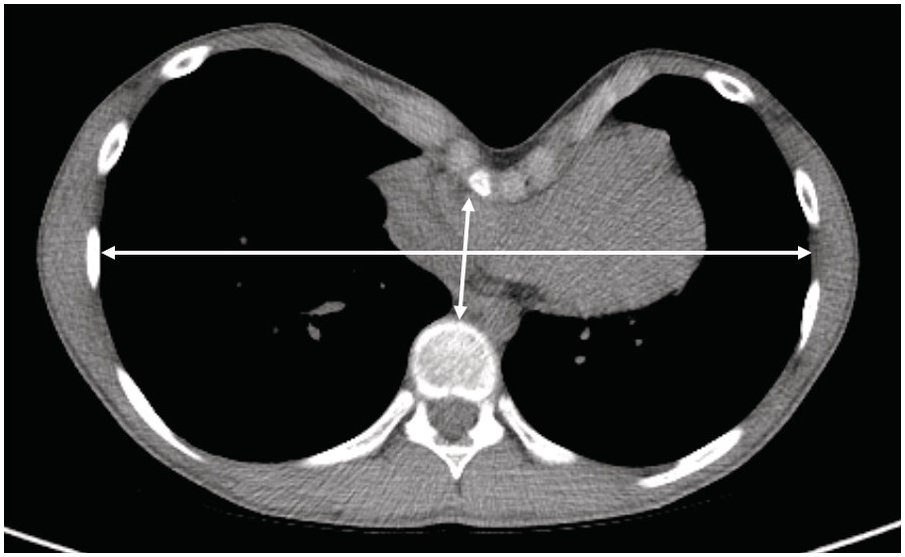
The diagnosis of this condition is made by clinical examination and inspection of the chest. To better define the defect and characterise the severity, it is also important to undertake a chest CT or chest MRI to be able to calculate the Haller index, which is an index of the severity of the pectus and which expresses how sunken the sternum is compared to the width of the rib cage. Some children and adolescents with symptoms of breathlessness, chest pain or reduced physical fitness may require further investigations like, for example echocardiogram (ultrasound scans of the heart), ECGs, and lung function and exercise tests with measurements of their breathing gases during the test. In some cases, the pectus might be associated also with abnormality of the spine, the most commonly observed being scoliosis.
Why children with pectus excavatum require cardiac assessment?
Whereas previously, several years ago, children and families were concerned about the cosmetic appearance of the chest, it haw becoming clear that there are also some functional consequences of sunken chest. Several children describe breathlessness and chest tightness when exercising, particularly for high levels of exercise. There has been a considerable deal of research to try to understand what the causes of that are. For example, it is known that children with significant pectus excavatum may have a slight displacement of the heart into the left chest as well a higher pressure applied to the outside surface of the heart. This can compromise how well the heart fills with blood when relaxing and can affect they way the heart functions during exercise. Additionally, there is evidence that the blood flow-split between the left and the right lung can be abnormal in people with significant pectus excavatum. When patients are formally exercise tested, it is not uncommon to see that the amount of air that they are breathing with every breath seems to reach a peak earlier than usual during exercise and subsequently seems to plateau early and not increase further as exercise continues. For those children, the only way to continue to exercise and to avoid stopping exercising is to increase their breathing rate up to levels often exceeding 50-55 times per minute, explaining the intense breathlessness described by many children and adolescents during exercise. There is evidence that treatment of this condition can lead to a significant improvement in the symptoms.
What treatment is required for pectus excavatum?
Many children and adolescents with mild pectus excavatum do no require any treatment. For those with more pronounced pectus, the treatment will vary depending on the age of the child or adolescent and the symmetrical or asymmetrical appearance of the chest. Whereas exercises and physiotherapy might be sufficient for children with mild pectus, other options including suction bells and ultimately surgical intervention might be required in children with more significant pectus. It is important to report that besides achieving a cosmetic effect, treatment is often also able to determine improvement in the functional capacity so that many children and adolescents feel they can exercise more and they feel less breathless during exercise.


